Male studies
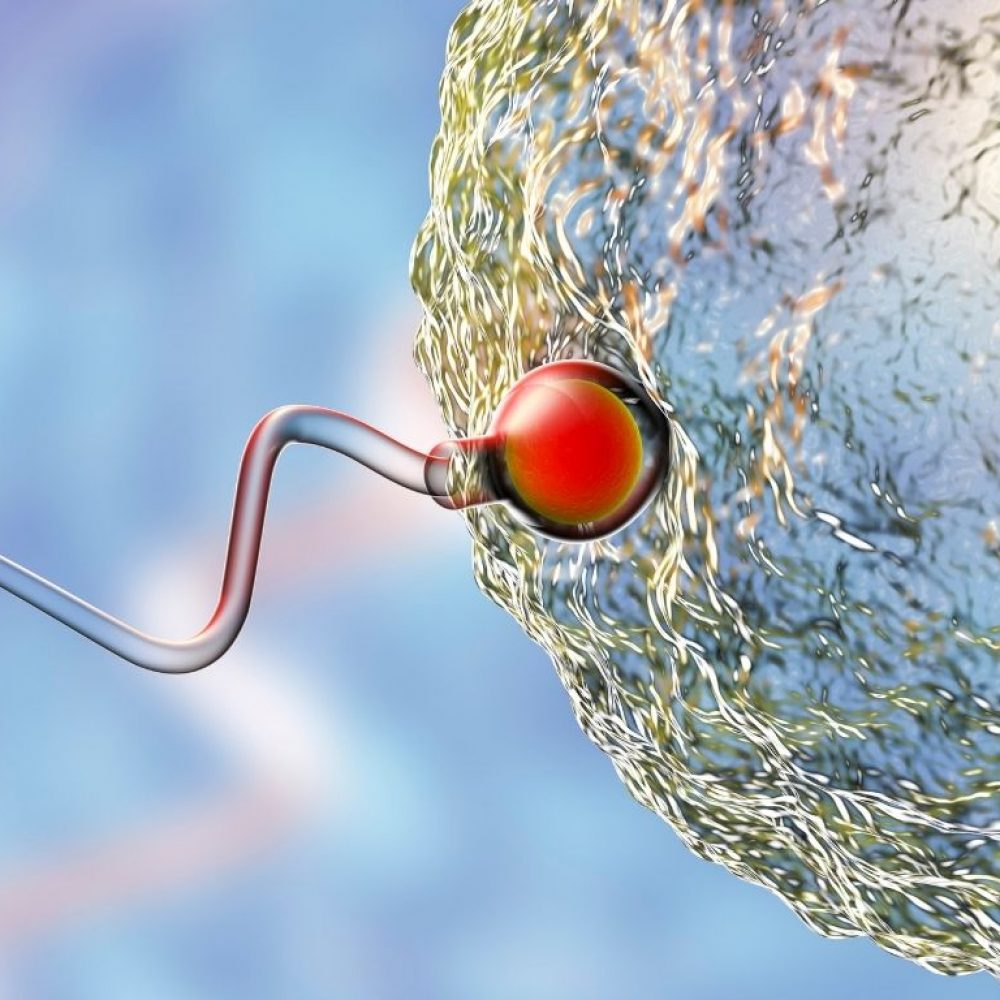
In the diagnosis of male infertility, sperm analysis, or spermogram is of the utmost importance. In the course of the examination, the count, motility and morphology of the sperm is assessed. Hormone tests are also important in assessing male fertility, while the presence of sexually transmitted diseases must be ruled out.
Genetic research into the causes of infertility has developed rapidly in recent times, and it has been proven that gene and chromosome mutations can cause infertility in both women and men.